Procedures
Depending on your specific weight condition, body type and end goals, there are a few different bariatric surgery options available to you. Each of these procedures comes with risks and benefits, and not everyone will be a candidate for every type of surgery. It is important that you discuss these procedures with your doctor in order to make an informed decision that will be the most beneficial to you and your long-term health.
Types of bariatric procedures for weight loss
Depending on your specific weight condition, body type and end goals, there are a few different bariatric surgery options available to you. Each of these procedures comes with risks and benefits, and not everyone will be a candidate for every type of surgery. It is important that you discuss these procedures with your doctor in order to make an informed decision that will be the most beneficial to you and your long-term health.
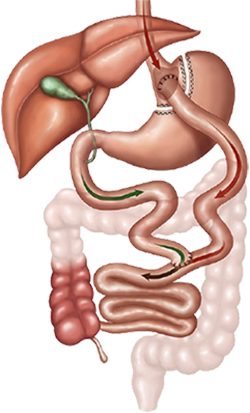
There are two components to gastric bypass surgery: shrinking the stomach size and rerouting food so that it reaches the small intestine faster. First, a small pouch is created in the stomach that can only hold a small amount of food before you feel full. This pouch is then strategically placed so that food bypasses the rest of the stomach and delivers food to the small intestine faster. By bypassing the stomach and parts of the small intestine, your body absorbs less fat and fewer calories. Be aware, however, that this also means your body will absorb fewer nutrients as well.
Service is available across Trinity Health Mid-Atlantic region.
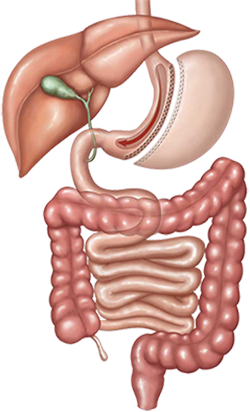
Sleeve gastrectomy, or vertical sleeve gastrectomy (VSG), is one of the most popular weight-loss surgeries. This procedure creates a thin sleeve of stomach by using a stapling device, and removal of the rest of the stomach. The sleeve is about the size of a banana and limits the amount of food you can eat which helps you feel full sooner. This results in fewer calories being consumed due to a reduced amount of food you can eat.
Service is available across Trinity Health Mid-Atlantic region.
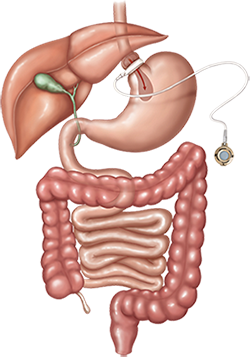
Adjustable gastric banding is a restrictive type of weight loss surgery, meaning it works by making your stomach "smaller." It involves placing an inflatable silicone band around the upper stomach to restrict food intake. Banding of the stomach does not affect digestion or absorption. Food should still pass through your system as usual, except you will not feel hungry as often. The band can be tightened or loosened over time to change the size of the passage. Gastric banding is a highly effective surgical option because it introduces you to new dietary habits.
Service is available at Mercy Bariatrics and Saint Francis Bariatric Surgery.
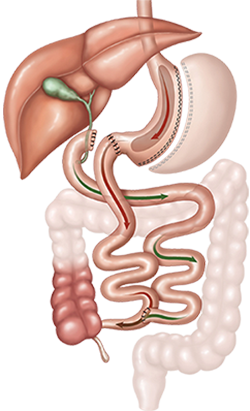 Biliopancreatic Diversion with Duodenal Switch (BPD/DS) is another form of gastric bypass. The first part of the procedure is a sleeve gastrectomy, where a small tube-like pouch is created in the stomach by removing the rest of the organ. Then the bypass procedure is performed, wherein the stomach reroutes food from the stomach down towards the end of the small intestine. The amount of small intestine bypassed in this procedure is significantly more than that in the Roux-En-Y gastric bypass. Skipping so much of the stomach changes the way food is digested by enzymes in the stomach, cutting back on your total calorie count.
Biliopancreatic Diversion with Duodenal Switch (BPD/DS) is another form of gastric bypass. The first part of the procedure is a sleeve gastrectomy, where a small tube-like pouch is created in the stomach by removing the rest of the organ. Then the bypass procedure is performed, wherein the stomach reroutes food from the stomach down towards the end of the small intestine. The amount of small intestine bypassed in this procedure is significantly more than that in the Roux-En-Y gastric bypass. Skipping so much of the stomach changes the way food is digested by enzymes in the stomach, cutting back on your total calorie count.
This procedure can reduce the absorption rate of fat by 70% or more. While it is effective, it also cuts down on the nutrients your body can absorb. You will need to speak with your doctor about how to maintain good nutrition after the operation.
Service is available at Saint Francis Bariatric Surgery and Mercy Bariatrics.
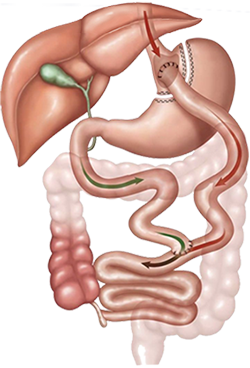 The duodenal switch surgery reduces the stomach using a stapling device, then attaches a section of the small intestine to the duodenum. The excised, unused portion of the stomach is removed. This allows food to bypass much of the small intestine, where calories and nutrients are normally absorbed. Typically patients lose about 70-80% of their excess weight following surgery.
The duodenal switch surgery reduces the stomach using a stapling device, then attaches a section of the small intestine to the duodenum. The excised, unused portion of the stomach is removed. This allows food to bypass much of the small intestine, where calories and nutrients are normally absorbed. Typically patients lose about 70-80% of their excess weight following surgery.
Service is available at Nazareth Bariatrics and Mercy Bariatrics.
Bariatric surgery is usually very successful; however, some patients may not succeed in losing the expected amount of excess weight. In these situations, a follow-up bariatric procedure, known as a bariatric surgery revision, may be necessary to alter or repair the initial bariatric surgery.
The OverStitch™ Endoscopic Suturing System enables the physician to revise a dilated gastric pouch or outlet to its original size. Full thickness sutures ensure tissue approximation is maintained until tissue is healed.
Service is available across Trinity Health Mid-Atlantic region.

