Every minute matters: Knowing the signs of stroke during American Stroke Month
May 20, 2025Categories: Blog Posts
Tags: Stroke
 Stroke is the fifth leading cause of death and one of the most common reasons for disability in the United States. However, stroke doesn’t always have to be fatal or force a person to live with long-lasting effects.
Stroke is the fifth leading cause of death and one of the most common reasons for disability in the United States. However, stroke doesn’t always have to be fatal or force a person to live with long-lasting effects.
During American Stroke Month, which takes place each May, Brad Bendesky, MD, chair of emergency medicine at Mercy Fitzgerald Hospital, and Barbara Tribuiani, BSN, RN, stroke and sepsis coordinator, are reminding community members that every minute counts when it comes to stroke care. It’s important to know how to recognize early symptoms, seek immediate help and engage in healthier lifestyle choices to lower—or eliminate—risk of stroke before it happens.
Mercy Fitzgerald Hospital, a Primary Stroke Center, treats the two main types of stroke: ischemic and hemorrhagic. Ischemic strokes take place more frequently, with most patients exhibiting the “classic” symptoms of weakness on one side of the body, dizziness, facial droop and/or the inability to speak.
“A clot, either a clot that forms in place or a clot that travels from the heart, will lodge itself into one of the blood vessels in the brain, cutting off the blood supply to a specific portion of the brain, depending on which of the branches it’s formed in or has traveled to,” says Dr. Bendesky.
Hemorrhagic stokes occur when a blood vessel begins to leak, possibly from an aneurysm. The pressure of blood in the brain will create a dysfunction in that specific part of the brain.
Recognizing stroke symptoms
If not treated quickly, stroke can cause death or irreparable damage to the brain, resulting in paralysis, memory problems, difficulty swallowing, behavioral changes and more. Being able to recognize early stroke symptoms, either in yourself or a loved one, is key to avoiding such damage.
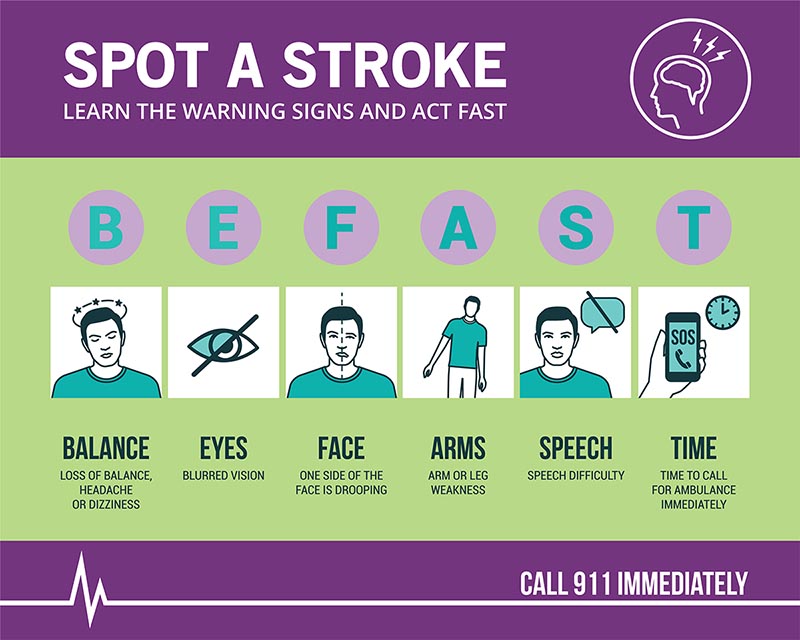
Tribuiani stresses the importance of the acronym BEFAST: Balance (sudden difficulty walking or standing upright), Eyes (loss of vision in one or both eyes), Face (facial drooping or twisting), Arm (numbness or weakness in the limbs), Speech (trouble speaking) and Time (call 911 immediately).
“They come in too late a lot of the time,” says Tribuiani. “We want people to know that these are the symptoms. Please don’t go to bed and wake up several hours later not able to get any help. That’s what happens a lot of time, where they wait two or three days. It’s awful.”
Patients may experience a mini stroke, or transient ischemic attack. During a TIA, a clot forms and cuts off a blood or oxygen supply to a portion of the brain, but it breaks up spontaneously, leaving the brain intact. Even if only minor symptoms are briefly felt, such as slight dizziness, the patient should still get checked out.
“Please don’t go to bed and wake up several hours later not able to get any help. That’s what happens a lot of time, where they wait two or three days. It’s awful.” — Barbara Tribuiani, BSN, RN
“It’s challenging sometimes because by the time the patient gets to us, the symptoms are gone. I use an analogy with patients all the time. When your car’s making the noise, you bring it to the shop and then it’s not making the noise when you get there,” says Dr. Bendesky. “But that doesn’t mean we don’t put you up on the rack and look at everything. We still have a way to find evidence that something bad did happen. Now we need to address those risk factors.”
Addressing risk factors for stroke
According to Dr. Bendesky, regular health maintenance visits with a primary care doctor are the best way to identify risk factors for stroke. These include atrial fibrillation, or an irregular heartbeat, which makes a patient more likely to form clots within the heart that can be released into the circulatory system and brain, causing a stroke.
“And certainly things like diabetes, high blood pressure and high cholesterol, which all contribute to vascular disease and plaques along your blood vessels,” says Dr. Bendesky. “These plaques are like having pipes that get clogged up. Cholesterol plaques will accumulate on the sides of the blood vessels and if they stay there, you might have slightly decreased blood flow through that pipe that is now a little bit clogged. But if one of those plaques ruptures, then it sends the clot into your body. If it lodges in your brain, you’ll have a stroke.”
Getting diabetes, high blood pressure and high cholesterol under control, especially among older patients, greatly reduces risk of stroke. A healthy diet, exercise and decreased salt intake also helps significantly.
“The patients that we talk to who have had strokes and we have not been able to reverse those deficits, a lot of them will say, ‘I wish I would have done this earlier’,” says Dr. Bendesky. “Their life is forever changed because they are dependent. Some of them cannot walk alone, some of them cannot talk. It affects every aspect of their life. So, this is a good month to remind everyone to just practice good health maintenance.”
Stroke care at Mercy Fitzgerald Hospital
As a Primary Stroke Center, Mercy Fitzgerald Hospital has a dedicated stroke unit that’s staffed with a clinical stroke team. When a possible stroke patient comes through the doors, doctors and nurses act quickly to assess their symptoms, call a stroke alert if warranted and immediately move them to a CAT scan, which can rule out or find a bleed.
“The patients that we talk to who have had strokes and we have not been able to reverse those deficits, a lot of them will say, ‘I wish I would have done this earlier’. Their life is forever changed because they are dependent. Some of them cannot walk alone, some of them cannot talk. It affects every aspect of their life. So this is a good month to remind everyone to just practice good health maintenance.” — Brad Bendesky, MD
The ED physician then consults with neurology to determine if the patient is within the window (4 and a half hours from the onset of symptoms) to receive thrombolytics, a clot-busting medication, or have the clot removed surgically (this would require a transfer to a nearby hospital).
The ability to salvage brain tissue in stroke patients has significantly improved over the past decade, especially when it comes to ischemic strokes.
“Twenty-five years ago, the imaging technology and the catheter-directed treatment therapy was not advanced enough to identify that the clot is in a very specific spot effecting this part of the brain,” says Dr. Bendesky. “The images are now so good that, once we know it’s not bleeding, we have thrombolytic therapy and we can actually put clot-busting medications into an IV and, hopefully, start to break up that clot to allow blood to flow to that area.”
